
The effect of pre-existing conditions on the progression of COVID-19
The COVID-19 pandemic has shown that there is a lot of variation in how people react to a SARS-CoV-2 infection. While some experience very few symptoms or even none at all, others become seriously ill. As a team led by Dr. Stefanie Kreutmair has now demonstrated, pre-existing conditions – particularly those affecting the kidneys – can be an indication of potentially severe cases of COVID-19.
Contact
Professor Burkhard Becher
Institute of Experimental
Immunology at the
University of Zurich
+41 44 635 37 03
E-Mail
UMZH institutions
University of Zurich
University Hospital Zurich
Team
>
No let-up in the virus
It’s summer 2022 and numbers of new coronavirus cases are rising, once again putting more pressure on hospitals and health authorities. Demand for scientific knowledge is also greater than ever. Ever since the start of the pandemic, research teams at the University of Zurich’s Institute of Experimental Immunology have been working flat out on investigating the effects of SARS-CoV-2 infections on the human immune system. What they are actually aiming to do is generate new findings to help hospital physicians responsible for treatment. After all, this virus is showing no signs of letting up.
This alliance between fundamental research and clinical practice has already started to bear fruit over the past year. Within a very short time, researchers at the University of Zurich made a vital breakthrough in combating COVID-19 by identifying a biomarker that can indicate severe cases of the disease even as soon as patients are admitted to hospital. In this case, the biomarker turned out to be specific T-cells in the blood – a particular class of white blood cells.

Where everything began at the start of 2020.
Immune cells fight off invaders
However, the body’s defensive response to COVID-19 varies from person to person, as different individuals have different levels of the special T-cell in their blood. These immune cells usually fight off invaders by, for example, killing off infected cells. Some COVID-19 patients have very few of these T-cells, which points to a problem with their immune defense. This can mean they end up becoming seriously ill with the virus. A team led by Professor Burkhard Becher and Dr. Stefanie Kreutmair at the University of Zurich’s Institute of Experimental Immunology, in collaboration with researchers from Tübingen, Toulouse and Nantes, first discovered this link back in mid-2021.
Kidney disease increases risk
Stefanie Kreutmair is a medical specialist in internal medicine, hematology and oncology at University Hospital Zurich and is equally at home in fundamental research and clinical practice. With the help of her team, she has now – halfway through 2022 – made even further progress. «During the pandemic, we have seen that elderly patients and those with certain pre-existing conditions generally become more seriously ill with the virus than others,» she says. «This prompted us to investigate whether these people not only have a lower level of special T-cells, but also develop another kind of immune response owing to their pre-existing condition.»
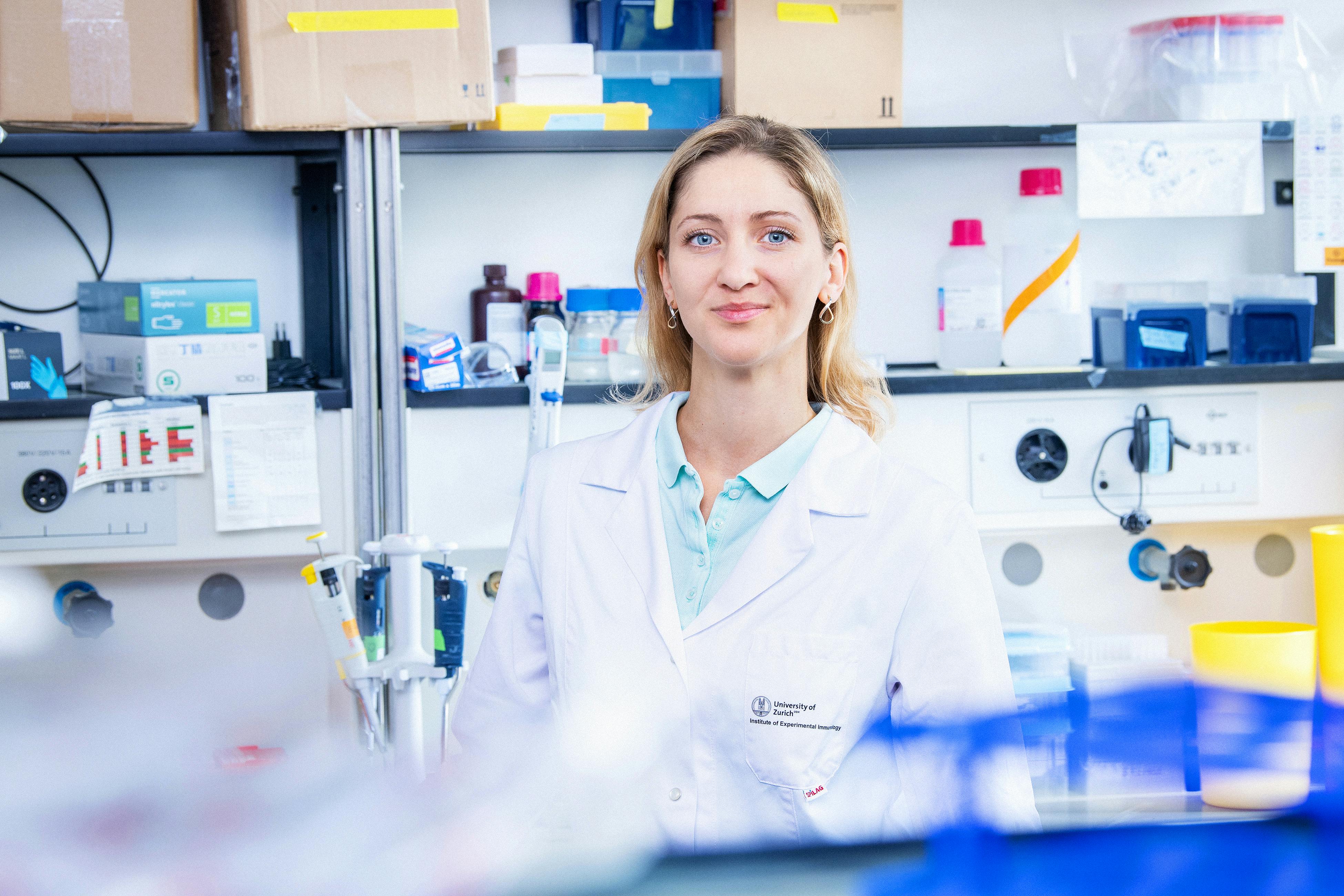
Recognition for her COVID-19 research: Stefanie Kreutmair was awarded the 2022 Theodor Frerichs Prize.
Using computer-aided analyses, Kreutmair and her team were able to evaluate data from over 50 COVID-19 patients and 121 samples to prove that people with kidney disease were at a significantly higher risk of developing severe COVID-19 than others. This level of risk was sixteen times higher than for patients with no pre-existing diseases and eight times higher than for those with a different pre-existing condition. «We identified typical immune signatures that are associated not just with severe cases of COVID-19, but also with pre-existing conditions,» Kreutmair explains. This was a pioneering breakthrough, as it marked the first time that this phenomenon had been demonstrated with such clarity. As Kreutmair also points out, the better we can understand and interpret the immune system’s individual warning signals, the more we can target our response to them. These findings have a direct practical relevance for specialists involved in treating the people affected. They can spot the warning signs as soon as a patient comes into their hospital and take appropriate measures based on this.
Award-winning work
In May, Stefanie Kreutmair was awarded the 2022 Theodor Frerichs Prize for her work on analyzing the immune signatures of COVID-19 patients. This prestigious accolade is worth EUR 30,000.
Link to new study by Dr. Stefanie Kreutmair

Burkhard Becher with his team on the Irchel Campus in Zurich (from left to right: Carla Helena Merten, Jonas Schmid, Susanne Unger, Jenny Kienzler, Stefanie Kreutmair, Burkhard Becher, Laura Power, Aakriti Sethi, Maximilian Schaefer, Nicolás Gonzalo Núñez, Sinduya Krishnarajah. Absent: Chiara Alberti, Sara da Costa Pereira, Florian Ingelfinger, Donatella De Feo, Dimitri Anderfuhren, Juan Manuel Villar Vesga, Tobias Wertheimer).
How do different vaccines work?
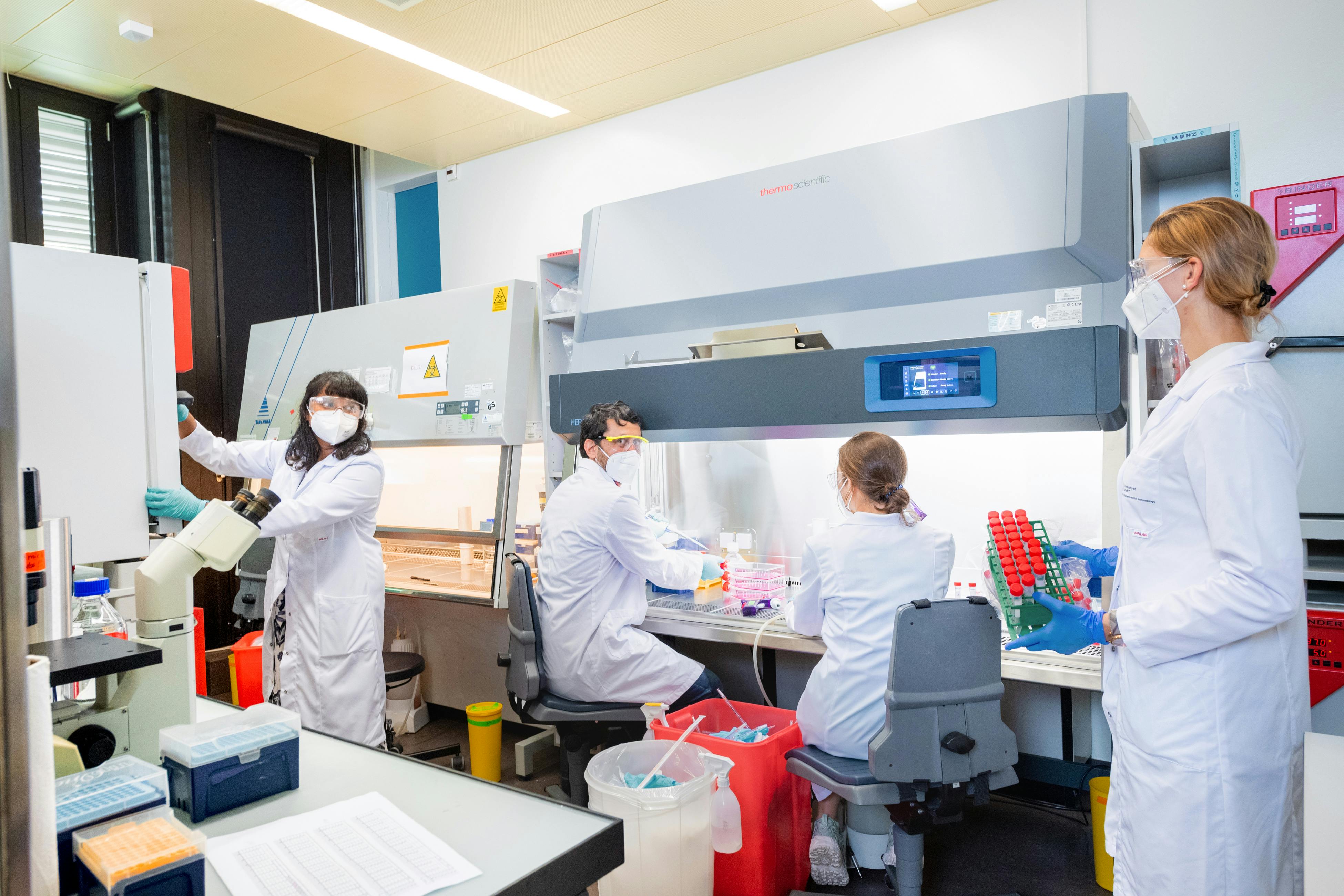
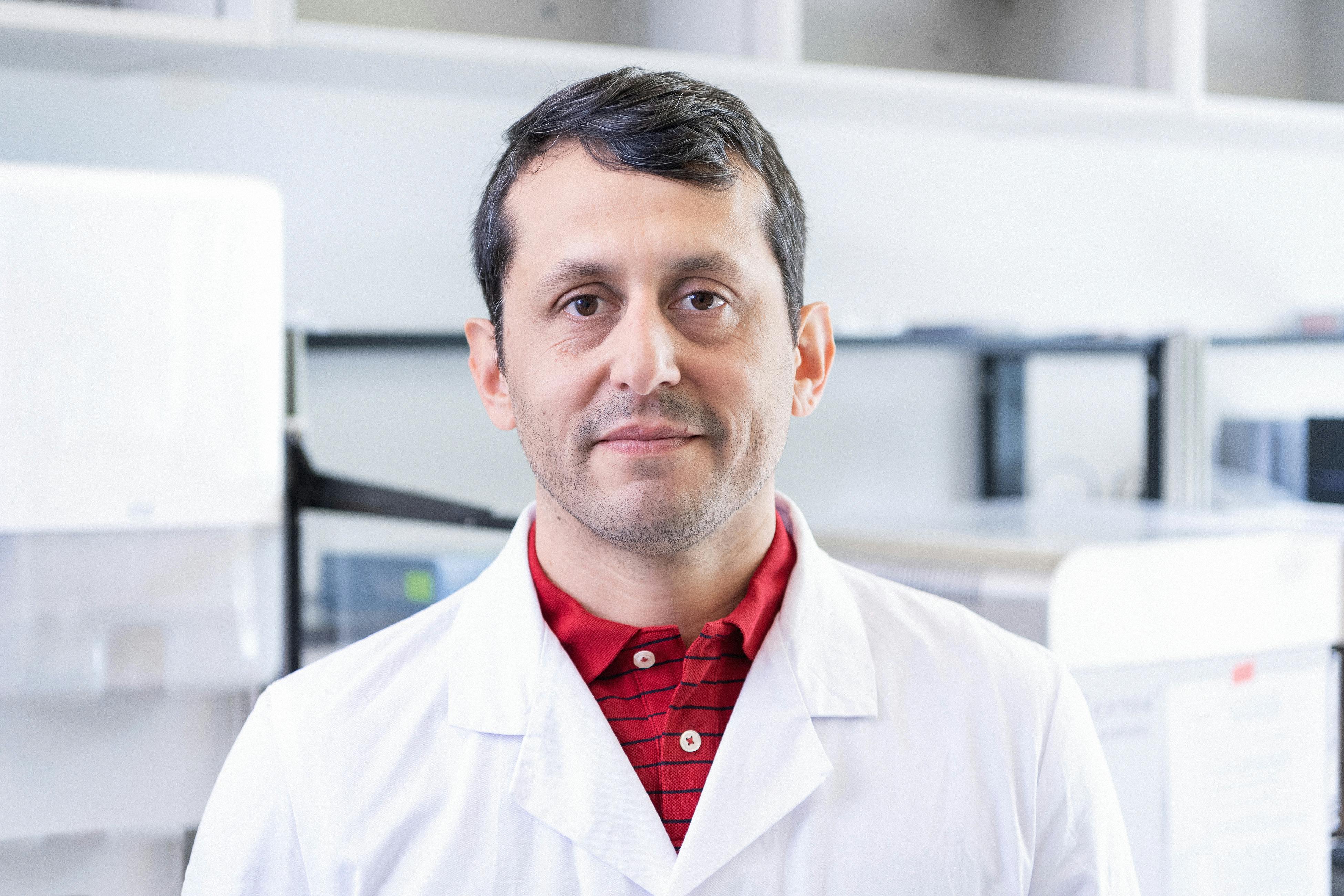
Immunologists Dr. Nicolas Nunez and Jonas Schmid, who are both part of Burkhard Becher’s team at the University of Zurich’s Institute of Experimental Immunology and have been conducting research with Stefanie Kreutmair, are working on another strand of immune research: they want to understand the ways in which the immune system responds to vaccines.
The researchers were lucky enough to gain access to data from Argentina, where several COVID-19 vaccines had already been approved at the time. Since Nunez works with researchers at the National University of Córdoba in Argentina, he was able to gain permission from the local health authority to analyze samples from vaccinated people for research purposes. This meant that, from as early as December 2021, he had access to blood samples from around 500 Argentinian patients who had been immunized with vector-based, mRNA or inactivated vaccines.
«We have a solid database containing a total of 800 samples of first and second vaccinations,» say the two immunologists. There are sixteen combinations overall, some of which involve different vaccines being used for the first and second dose. Nunez and Schmid are now analyzing the samples at single-cell level with the help of flow cytometry. They then use computer algorithms to evaluate the data, drawing on support from bioinformatician Laura Power. The researchers are expecting to gain new findings that could have a significant influence on future vaccination strategies.

Laura Power, Nicolás Gonzalo Núñez, and Jonas Schmid (from left to right) analyse the effectiveness of different vaccines.






Listen
Stefanie Kreutmair (Audio file in German, July 2022)
«People with chronic kidney disease seem to be at particularly high risk»
Dr. Stefanie Kreutmair is a medical specialist in internal medicine, hematology and oncology at University Hospital Zurich and is leading the research project at the Institute of Experimental Immunology at the University of Zurich.

Nico Nunez (July 2022)
«Our cohort for this vaccine study is unique»
Dr. Nico Nunez is a postdoctoral researcher at the Institute of Experimental Immunology at the University of Zurich.
Jonas Schmid (Audio file in German, July 2022)
«We want to know how the immune system responds to different vaccines»
Jonas Schmid is a doctoral student at the Institute of Experimental Immunology at the University of Zurich.

Burkhard Becher (Audio file in German, July 2021)
«We have succeeded in identifying the targets for treatment»
Professor Burkhard Becher is a professor at the Institute of Experimental Immunology at the University of Zurich.

Stefanie Kreutmair (Audio file in German, July 2021)
«I wanted to contribute to the fight against the pandemic»
Dr. Stefanie Kreutmair is a specialist in internal medicine, hematology, and oncology at University Hospital Zurich and is heading the research project at the Institute of Experimental Immunology at the University of Zurich.

Chiara Alberti (July 2021)
«Our results show how important it is to tailor the treatment to each individual patient»
Dr. Chiara Alberti is a postdoctoral researcher at the Institute of Experimental Immunology at the University of Zurich.
Nico Nunez (July 2021)
«We have worked with patient samples from various European countries»
Dr. Nico Nunez is a postdoctoral researcher at the Institute of Experimental Immunology at the University of Zurich.
Susanne Unger (Audio file in German, July 2021)
«We wanted to be able to predict serious cases of COVID-19 from blood samples»
Dr. Susanne Unger is a postdoctoral researcher at the Institute of Experimental Immunology at the University of Zurich.
Service
Long COVID: Clinic at University Hospital Zurich
Individual risk for Long-COVID: A research group led by Professor Onur Boyman, Director of the Department of Immunology at University Hospital Zurich, developed a model to calculate the personal risk of developing Long COVID. (The test requires that certain blood measurements are known, e.g. blood immunoglobulin level)
University Hospital Zurich: COVID test and vaccination
University Children's Hospital Zurich: COVID test and COVID vaccination
Glossary
Biomarkers:
These are measurable parameters of biological processes that can be used for prognostic or diagnostic purposes and therefore function as indicators of diseases, for example. They are characteristic biological features that can be measured objectively and can indicate a normal biological process or a disease in the body. Biomarkers can be cells, genes, gene products, or specific molecules, such as enzymes or hormones.
Flow cytometry:
Flow cytometry (cytometry = the measurement of cells) is a measuring technique used in biology and medicine. It makes it possible to analyze individual cells as they flow by at high speed using an electric voltage or a beam of light.
Hematology:
The study of blood and its components..
SARS-CoV-2:
The coronaviruses are a family of viruses that can cause various diseases. Seven different coronaviruses have so far been identified in humans. The current coronavirus is officially known as SARS-CoV-2. The illness caused by a SARS-CoV-2 infection is called COVID-19.
Vector-based vaccine:
Genetic information from the virus is inserted into harmless adenoviruses (vector = carrier). These trigger an immune response in the body, but do not cause illness.
mRNA vaccine:
Only fragments of the genetic virus material, the messenger RNA, are injected. Human cells read the messenger RNA and use it to create their own virus components. The immune system then reacts to these components and creates antibodies.
Inactivated vaccine:
Inactivated vaccines are made from deactivated pathogens. The body recognizes them as foreign objects and creates antibodies in defense.
Who is co-financing this project? (in CHF millions)
The LOOP Zurich - Medical Research Center
Vontobel-Stiftung
The project funding lasts from 2020 to 2022
Credits
Text and audio: Rebekka Haefeli, Marita Fuchs
Pictures: Frank Brüderli
University of Zurich: Stefanie Kreutmair, Burkhard Becher, Nicolás Gonzalo Núñez, Susanne Unger, Sinduya Krishnarajah, Florian Ingelfinger, Carla Helena Merten, Jonas Schmid, Jenny Kienzler, Laura Power, Aakriti Sethi, Sara da Costa Pereira, Donatella De Feo, Dimitri Anderfuhren, Juan Manuel Villar Vesga, Tobias Wertheimer
The LOOP Zurich - Medical Research Center: Jens Selige





