Precision medicine to combat obesity
Many overweight and obese people are constantly battling to lose those extra pounds – often in vain. There is a distinct lack of new therapies targeted toward individuals and their personal circumstances. The LOOBesity project is eager to change this, and is adopting an approach to weight loss based on precision medicine. It aims to make the fight against obesity and the diseases associated with it more effective and better tailored to individual needs. The researchers are playing particularly close attention to the role of the stress hormone cortisol.
Contact
Prof. Dr. Felix Beuschlein
Head of Clinic at the Department of Endocrinology, Diabetology and Clinical Nutrition at University Hospital Zurich
+41 44 255 36 25
E-Mail
UMZH institutions
University of Zurich
University Hospital Zurich
ETH Zurich
Team
Margrit M.* slowly makes her way up the stairs leading to the main entrance of University Hospital Zurich (USZ). The 63-year-old has a body mass index (BMI) of 32, which puts her in the «obese» category, not the «overweight» category, as the cut-off value for the latter is 30. People with a BMI of between 18.5 and 24.9 are considered a healthy weight. Those extra pounds make it harder for her to climb the stairs and cause her to suffer from knee pain. Margrit M. is a patient of Privatdozent Philipp Gerber, Chief of Service at the Department of Endocrinology, Diabetology and Clinical Nutrition at University Hospital Zurich. During his specialist consultations, Gerber and his team endeavor to help patients lose weight by encouraging them to make changes to their diet and nutrition, offering exercise therapy and treating them with medication. Yannik W.* is also a patient here. The 40-year-old nurse works shifts. His weight has steadily increased since his training days and, with a BMI of 35, he now falls into the «morbidly obese» category. Yannik W. really wants to lose weight and has tried many different diets over the years, but the famous yo-yo effect has dashed all his hopes.
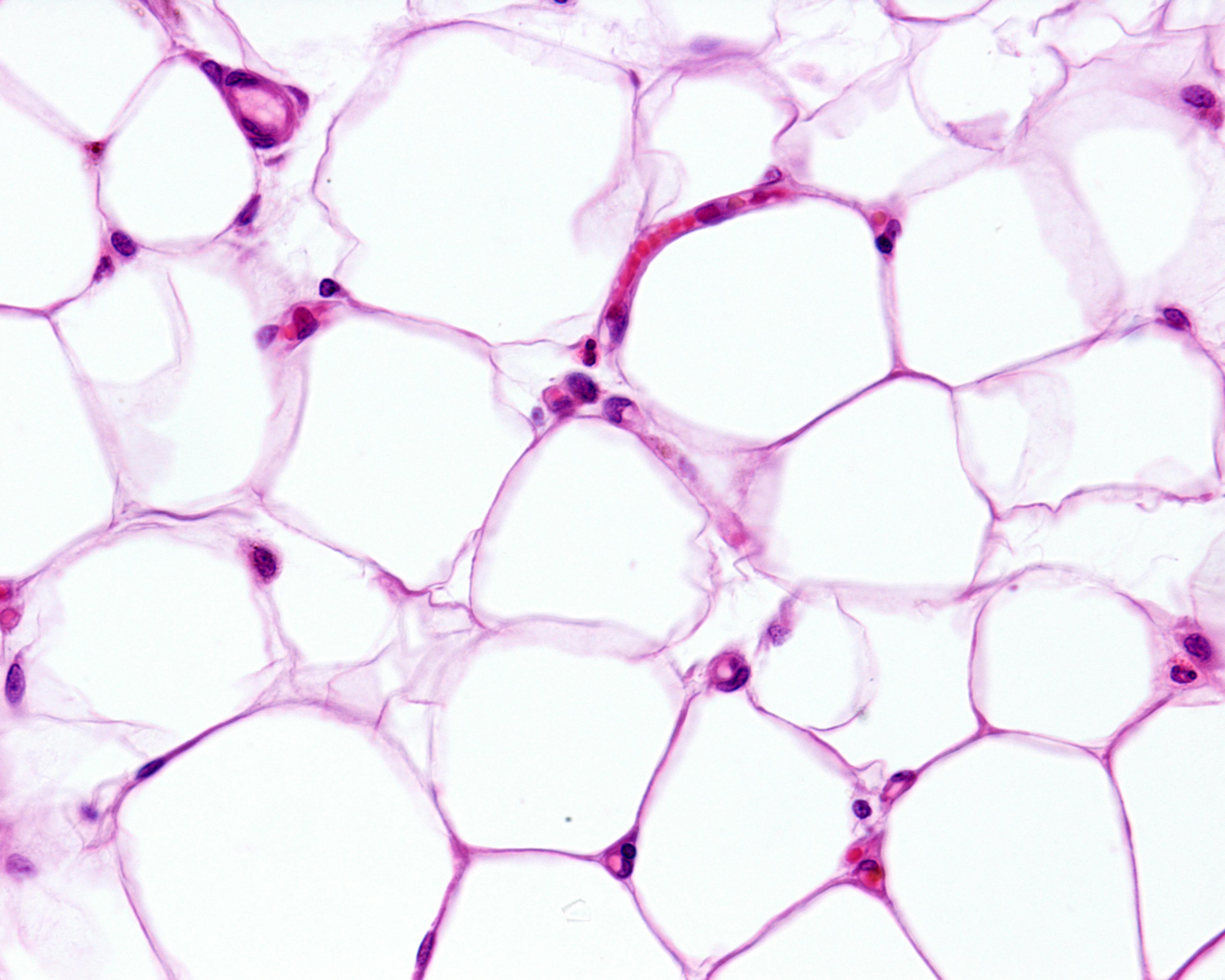
Both Yannik and Margrit signed up to take part in the «Zürcher Adipositas Kohorte» (Zurich Obesity Cohort) project, which collects patient data, and have now also been accepted as participants in the new «LOOBesity» project. They agreed to provide regular updates about the state of their health, have a biopsy taken of their adipose tissue, and undergo a magnetic resonance imaging (MRI) scan. All in all, more than 300 overweight and obese patients are set to participate in the study as part of the «LOOBesity» research project. The project is still in its very early stages, having been launched in 2023. All health data will be collected and evaluated by researchers throughout the year, with initial results expected at the end of the year. Once the cohort study has been concluded, a randomized study is in the pipeline for next year (see glossary).
Interdisciplinary team of researchers
The name «LOOBesity» is an amalgamation of «The LOOP Zurich», the translational research center dedicated to precision medicine and obesity. «We are adopting a precision medical approach to weight loss under the auspices of the LOOP Zurich,» says Milo Puhan, Director of the Epidemiology, Biostatistics and Prevention Institute at the University of Zurich. «We want to use the cohort study to find out how and for whom specific therapies and medicines work,» adds Felix Beuschlein, Head of Clinic at the Department of Endocrinology, Diabetology and Clinical Nutrition at University Hospital Zurich. The project’s interdisciplinary team is made up of Milo Puhan, Felix Beuschlein, and Philipp Gerber, along with a team of researchers from University Hospital and ETH Zurich. The project is set to take place over five years and is being funded by various sources, including Academic Medicine Zurich (research group).
Marion S.* is also part of the current cohort. For many years now, she has had to take cortisone to treat her asthma, but this prolonged use has caused her to develop Cushing’s syndrome. People with Cushing’s syndrome are overweight – and most are obese. They tend to store fat primarily around the upper body, the stomach, and the hips, but their arms and legs are often noticeably thin due to muscle weakness. People with the condition also commonly suffer from comorbidities and are at greater risk of developing cardiovascular diseases.
Cortisol as a game changer
For Marion S. her Cushing’s syndrome was caused by the administration of cortisone. There are, however, people whose bodies produce too much cortisol, and they can also develop the disease. Cortisol is a hormone that has an important part to play in the regulation of carbohydrate, fat, and protein metabolism.
That is why the researchers are particularly interested in assessing the role of cortisol when analyzing tissue from the biopsies taken from participants in the cohort study. This stress hormone, which is produced by the adrenal glands, acts to raise the blood sugar. This excess blood sugar is then stored as fat, particularly in the abdominal area.
The researchers now hypothesize that reducing a person’s cortisol levels using medication will help them lose weight and thus have a positive impact on their comorbidities. However, it is not yet known what exactly happens in the fat cells and how cortisol actually affects a person’s health. «In most people, the fat cells bathe in a sea of cortisol, despite the fact that the levels detected in the blood aren’t elevated,» says Beuschlein. «Were we to find out that some patients respond well to medication that changes cortisol metabolism, this would be a major step in the direction of using precision medicine to treat obese and overweight patients.» However, it is not yet known exactly how metabolic processes work and who may or may not benefit from a drug-based approach to cortisol reduction.
Markers for tailored therapies
It is therefore important to develop a personal profile to determine future targeted treatments. «With the LOOBesity project, we want to gain a differentiated understanding of overweight and obese people and identify markers for tailored therapies,» explains Puhan. «This will allow us to provide treating physicians with guidance how to treat individual patients, and allow them to assess more accurately and at an earlier stage what might work for which patients in the future.»
The researchers are currently at the start of the project and are collecting data about the cohort. The data set, which comprises molecular details of the individual analyses of adipose tissue and cortisol concentrations as well as image data from MRI scans, is vast and is under analysis using artificial intelligence. «Clinical data, imaging, and the molecular characteristics of patients are being analyzed in detail, so that we can identify parameters that make the difference between healthy people and unhealthy persons who are overweight and obese,» explains Puhan. There are individuals who, despite being severely overweight, have very few metabolic and cardiovascular comorbidities. These people are considered metabolically healthy.
Gateway for countless diseases
However, obesity is generally seen as a sort of gateway for countless diseases. Many people experience the same issues as Margrit M., Yannik W., and Marion S.: Overweight people are often chronically sick, and go on to suffer from conditions like cardiovascular diseases, diabetes, asthma, high blood pressure, and cancer. Yet, in spite of all these negative factors, the number of overweight people has been increasing at an alarming rate in most countries for many years now. According to the World Health Organization (WHO), more than half of adults in Europe now weigh more than they should. In Switzerland, around 40 percent of the adult population is overweight, and around 11 percent is obese.
So why not just eat less? The physicians offering specialist consultations at University Hospital Zurich understand that it can be difficult for patients to change their habits. As Felix Beuschlein explains, a multimodal approach to treatment, comprising nutritional counseling, exercise plans, and medication or surgery, is now adopted as standard. But who benefits most from what? If medication is prescribed, some patients will see a benefit, while others will barely lose any weight or will experience severe side effects.
Maximum benefit, minimal drawbacks
Some medications that are being used today to combat obesity are not new – they are substances that have been utilized to treat patients with diabetes for quite some time. But what these medications all have in common is their active ingredient; a gut hormone called GLP-1. This helps to lower blood sugar levels after a meal by making the body secrete more insulin and less of its counterpart glucagon. The stomach empties more slowly and feelings of hunger are reduced. These medications – which are currently being hyped up – can, however, cause side effects such as nausea and intestinal complaints. Drugs used in people with diabetes can also lead to weight loss in overweight and obese individuals. However, these medications stop working as soon as a patient ceases taking them, and we still know very little about the undesirable effects associated with long-term use. Shedding light on this situation is a further aim of the LOOBesity project. In summary, the approach adopted here is based on a personalized therapy strategy that modulates the effect of cortisol, thereby providing patients with maximum benefit and minimal drawbacks in the treatment of obesity.
*Patients’ names changed
Listen
Ender Konukoglu
«Our algorithms identify disease activity in MRI images of adipose tissue»
Prof. Dr. Ender Konukoglu is an Associate Professor of Biomedical Image Computing at ETH Zurich.

Services
Obesity:
Center for Obesity and Metabolic Surgery, USZ
Glossary
Biomarkers:
Measurable parameters of biological processes in medicine that can be used for prognostic or diagnostic purposes, and therefore function as indicators of diseases, for example. They are characteristic biological features that can be measured objectively and can indicate a normal biological process or a disease in the body. Biomarkers can be cells, genes, gene products, or specific molecules, such as enzymes or hormones.
Body mass index:
Body mass index (BMI) is used as a reference value to assess a person’s weight in relation to their height. BMI is calculated by dividing body weight (kg) by height in meters squared (m2). BMI does not, however, take into consideration a person’s age or the distribution of body fat or muscle mass. Adults with a BMI of between 18.5 and 24.9 are considered a healthy weight. Those with a BMI over 25 are considered overweight, and over 30 are considered obese.
Cohort study:
In a cohort study, a certain group of people with certain common features – in the case described above, overweight and obese people – is observed over an extended period of time. The idea behind a cohort study is to track changes or developments in this group over time and to determine whether there is a relationship between the common features and certain results. By collecting data over time, researchers can uncover cause-and-effect relationships.
Metabolic:
This term is used to refer to the metabolism or the biochemical processes that occur in a living organism to produce energy, process nutrients, and maintain other vital functions.
Obesity:
A chronic nutrition-related and metabolic disorder. It is characterized by severe obesity resulting from an above-average increase in body fat.
Randomized study:
A research method that involves participants being assigned randomly to different groups. One group is an intervention group, which will undergo a certain treatment, measure, or condition, while the other group, the control group, will either receive no treatment or another standard treatment.
Who is co-financing this project? (in CHF millions)
The LOOP Zurich - Medical Research Center
The project funding lasts
from 2023 to 2028
Credits
Text: Marita Fuchs
Audio: Rebekka Haefeli
Pictures: Frank Brüderli
University of Zurich: Felix Beuschlein, Milo Puhan
University Hospital of Zurich: Felix Beuschlein, Nina Derron, Philipp Gerber
ETH Zurich: Ender Konukoglu
The LOOP Zurich - Medical Research Center: Jens Selige





